Patient Accounting Rep III
Job ID: R-39814
Job Type: Full time
Location: Lenexa, Kansas
Position Summary / Career Interest:
The Patient Accounting Representative III is responsible for functions within assigned Patient Financial Services (PFS) department. Responsible for accurate and timely action on accounts as it relates to specific responsibilities. Complies with governmental and managed care rules and regulations. Meet department goals as well as productivity and quality standards. Attends and actively participates in training and education.
The Patient Accounting Representative III is responsible for functions within assigned Patient Financial Services (PFS) department. Responsible for accurate and timely action on accounts as it relates to specific responsibilities. Complies with governmental and managed care rules and regulations. Meet department goals as well as productivity and quality standards. Attends and actively participates in training and education.
Responsibilities and Essential Job Functions
- Must be able to perform the professional, clinical and or technical competencies of the assigned unit or department.
- Responsible for coordinating the team’s workload and daily assignments
- Serves as a resource and provides training to staff in collaboration with supervisor. Serves as an Epic “super user” for area of responsibility.
- Conducts staff training or education specific to their department workflows including new hire orientation and facilitating lunch and learns as needed to assist the supervisor.
- Leads the team in the absence of the supervisor or upon assignment.
- Will be required to fill in for any Departmental needs as assigned.
- Responsible for other duties or projects which are assigned by Management. These may include special projects, telephone coverage, filing, copying and other duties as instructed.
- Reviews Research related charges, directing charges to the proper responsible financial payer source.
- Applies billing rules to research related charges billable to third-party health insurance payers based on CMS Claims Processing guidelines for Research Services.
- Invoices study billable services to the correct study and applying the standard applicable discount.
- Assists Study teams and the CTO in understanding of monthly invoices, answering questions and making corrections of any identified errors.
- Follows up with Study Groups on outstanding sturdy related billing and balances owed by the study.
- Assists with traditional follow up for Claims handled in the ""normal"" insurance billing/follow-up processes for Standard of Care services billed and followed up by the teams that follow up with insurance when questions arise regarding any impacts of billing related to the patient being in a clinical trial where traditional follow up is unable to remedy the denial.
- Posts payments, refunds and adjustments to accounts within designated time frame determined by workload.
- Completes assigned work queue within designated time frame determined by workload.
- Balances receipts, reconciles daily batches and prepares audit trail in accordance to department guidelines determined by workload.
- Reviews Explanation of Benefit’s for incorrect and or inconsistencies in reimbursement and resolves escalated EOB issues.
- Identifies consistent fee schedule allowable differences, resolves any differences, escalates and communicates up line for updating, and issues beyond their scope range.
- Observes and communicates payer trends to management.
- Develops new and creative methods for patient accounting rep staff to utilize performing day-to-day duties as problems or issues arise.
- Follows up with insurance companies on denials and insurance inquiries as necessary to resolve the account.
- Provides additional information or documentation as needed to resolve account.
- Notes actions taken on the accounts and verifies, and updates insurance as directed by department policy.
- Completes assigned work queue within designated time frame.
- Processes adjustments on accounts as necessary in compliance with department policy.
- Receives and resolves patient billing questions and complaints in a compassionate, courteous, professional and timely manner.
- Communicates with patients and de-escalates patient call situations that have been escalated by patient accounting rep II staff. Determines when to escalate a patient call to the supervisor or manager.
- Takes actions to resolve issues such as changing insurance, re-filing claims, calling and effectively communicating with insurance companies or answering questions.
- Documents actions taken as directed by department policy.
- Works closely with collection agencies to assure that they receive updated information on accounts.
- Coordinates the filing of liens as needed.
- Negotiates settlements with third parties as applicable.
- Must be able to perform the professional, clinical and or technical competencies of the assigned unit or department.
- These statements are intended to describe the essential functions of the job and are not intended to be an exhaustive list of all responsibilities. Skills and duties may vary dependent upon your department or unit. Other duties may be assigned as required.
Required Education and Experience
- High School Graduate or GED.
- 3 or more years of experience in payment posting, claims, denials, health care customer service, insurance processing, billing or collections.
Preferred Education and Experience
- Associates Degree in a related field of study from an accredited college or university.
- 4 or more years of Epic experience.
We are an equal employment opportunity employer without regard to a person’s race, color, religion, sex (including pregnancy, gender identity and sexual orientation), national origin, ancestry, age (40 or older), disability, veteran status or genetic information.
- Clinical Nurse Auditor - Rev Cycle Lenexa, Kansas
- Access Revenue Cycle Optimization Analyst Lenexa, Kansas
- Revenue Cycle Quality & Training Analyst (Access)-Hybrid Lenexa, Kansas
You don't have any recently viewed jobs yet. You don't have any saved jobs yet.
You don't have any recently viewed jobs yet. You don't have any saved jobs yet.
-
 All About Ambulatory Pharmacy
All About Ambulatory Pharmacy -
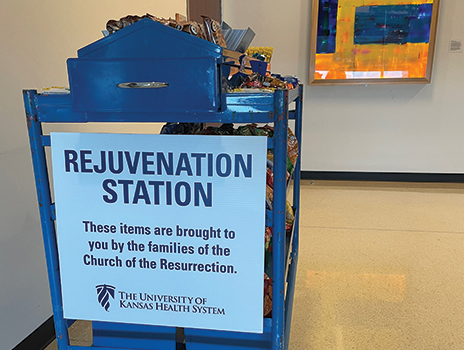
 Toby's Take: Caring for the Caregivers
Toby's Take: Caring for the Caregivers -
 Additional Clinical Opportunities
Additional Clinical Opportunities -
 Residency and Fellowship Programs Non-Nursing
Residency and Fellowship Programs Non-Nursing -
 A look into the life of an ER Nurse
A look into the life of an ER Nurse -
 Employee Testimonials
Employee Testimonials -
 Business & Professional
Business & Professional -
 Hospitality Services
Hospitality Services -
 IT
IT -
 Radiology
Radiology -
 Nursing
Nursing -
 Nursing Acute Care - Kansas City
Nursing Acute Care - Kansas City -
 Critical Care/ICU/ER
Critical Care/ICU/ER -
 Emergency - Great Bend
Emergency - Great Bend -
 Graduate Nurses/ Residency
Graduate Nurses/ Residency -
 Maternal and Child Services Division - Kansas City
Maternal and Child Services Division - Kansas City -
 Maternal and Child Services Division - Great Bend
Maternal and Child Services Division - Great Bend -
 Cancer Center
Cancer Center -
 Pathways to Nursing
Pathways to Nursing -
 Perioperative and Procedural Services - Kansas City
Perioperative and Procedural Services - Kansas City -
 Perioperative and Procedural Services – Great Bend
Perioperative and Procedural Services – Great Bend -
 Advanced Practice Professionals - Great Bend
Advanced Practice Professionals - Great Bend -
 Advancement Opportunities
Advancement Opportunities -
 Ambulatory & Outpatient - Kansas City
Ambulatory & Outpatient - Kansas City -
 Ambulatory & Outpatient
Ambulatory & Outpatient -
 Behavioral Health
Behavioral Health -
 Cardiovascular Care
Cardiovascular Care -
 Physicians & Faculty
Physicians & Faculty -
 Mission & Values
Mission & Values -
 Our Culture
Our Culture -
 Benefits
Benefits -
 Diversity & Inclusion
Diversity & Inclusion -
 History
History -
 Our Hiring Process
Our Hiring Process -
 Advanced Practice Professionals
Advanced Practice Professionals -
 Awards
Awards -
 Allied Health
Allied Health -

-

Our Hiring Process
Learn More -

Benefits
Learn More